In recent years, celebrities like Kim Kardashian have taken to social media to tout the supposed benefits of whole-body MRI scans. Companies that offer the service promise that the scans can spot a range of conditions, including cancer, aneurysms, liver disease and multiple sclerosis, in as little as an hour. And if the initial scan looks clear, the companies encourage clients to return periodically to check up on their health status.
But are full-body MRIs really a silver bullet, or just another expensive health fad?
According to Dr. Matthew Davenport, a professor of radiology at the University of Michigan, for most people, whole-body MRI scans aren’t only unnecessary but can actually lead to their own set of problems.
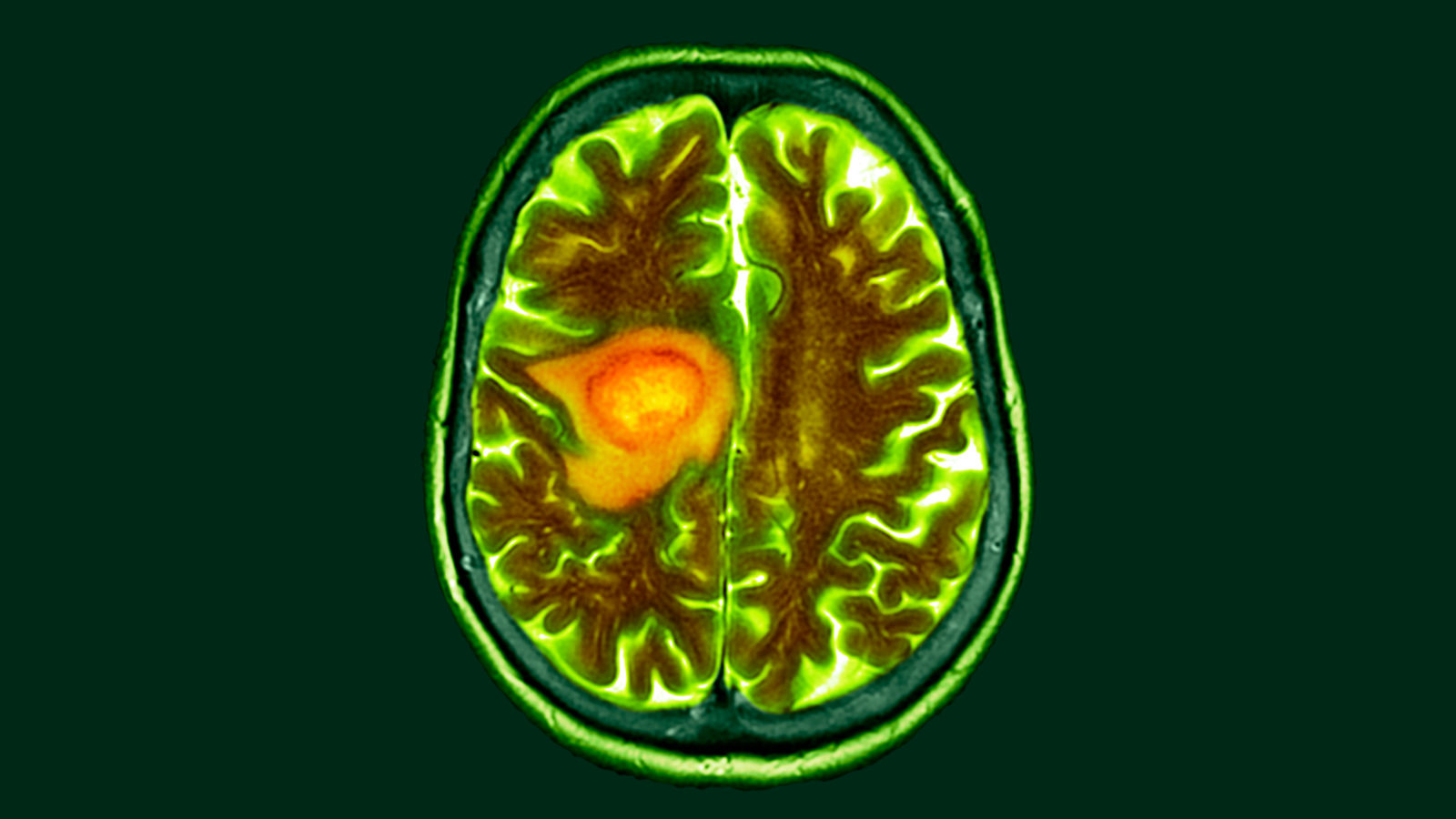
Structural MRI scans visualize the inside of the body using magnetic fields and radio waves. Because they render detailed 3D images of internal anatomy, they’re useful for detecting various conditions, including blood clots, musculoskeletal injuries, tumors, and neurological or cardiovascular problems. But doctors normally order these scans only when they already suspect that something is wrong based on an individual’s symptoms, medical history and other test results.
In some circumstances, doctors may recommend regular whole-body MRIs for certain patients as a preventive measure, Davenport said. But this generally occurs only when patients are diagnosed with rare disorders that put them at high risk of developing cancer. Such conditions include Li-Fraumeni syndrome, a genetic disorder that increases the risk of developing cancer at a young age.
The idea is that the regular scans could spot lesions in these high-risk individuals, potentially flagging them for further testing. However, for people without such conditions, there’s little reason to get regular full-body MRIs, Davenport said.
“There is no scientific evidence that whole-body MRI in asymptomatic, average-risk patients improves health,” he told Live Science in an email.
In fact, full-body MRIs may actually do more harm than good, he said. That’s because tests that can be used for diagnostics, like MRI scans, are likely to discover incidental findings.
Incidental findings are unexpected results that occur from a medical test ordered for a different reason. For example, a person might get an MRI of an injured rib and then have a suspicious mass pop up on the scan. Sometimes, these findings end up pointing to a previously undiagnosed condition that requires treatment. But more often, they’re just benign abnormalities in the body that pose no threat.
Related: The 10 deadliest cancers, and why there’s no cure
About 15% to 30% of diagnostic imaging tests raise at least one incidental finding, estimates suggest. That means people who get regular whole-body MRIs are likely to find abnormalities in their bodies that may not indicate any serious health issues.
“The vast majority of findings identified by whole body MRI in a patient without specific risk factors will be findings that would not improve health if they had not been detected,” Davenport said.
Nevertheless, you may not know if an incidental finding is important without further tests, so these results can prompt additional diagnostic tests, biopsy procedures and even unnecessary surgeries — not to mention the health anxiety that can accompany those procedures. Because of this, Davenport argues that ordering too many medical imaging tests on otherwise healthy people is likely to backfire.
Currently, no major medical societies recommend whole-body MRIs for people without conditions that put them at high risk of cancer. Davenport also pointed out that companies that offer full-body MRIs benefit from a highly profitable business model in that clients pay for the tests out-of-pocket.
Full-body MRIs typically cost anywhere from $1,000 to over $4,000, depending on the provider and specific service they’re offering. Some insurance plans may cover whole-body MRIs in high-risk individuals, but because the scans are elective for most and not backed by clinical guidelines, they’re generally not covered by private or government insurance in the U.S.
While on one hand, whole-body MRIs may stoke health anxiety and lead to potential overtreatment, in some people, they may also provide a false sense of security, Davenport suggested. For many medical conditions, such as colon cancer and blood cancer, MRIs aren’t used as a primary diagnostic tool because the scans don’t necessarily pick up the diseases. Davenport recommended that the general public stick with established medical screening procedures recommended by physicians rather than relying on whole-body MRI.
“It is possible we will see a future where imaging like whole body MRI is used for routine screening,” Davenport said. “However, substantial research is needed before that.”
This article is for informational purposes only and is not meant to offer medical advice.