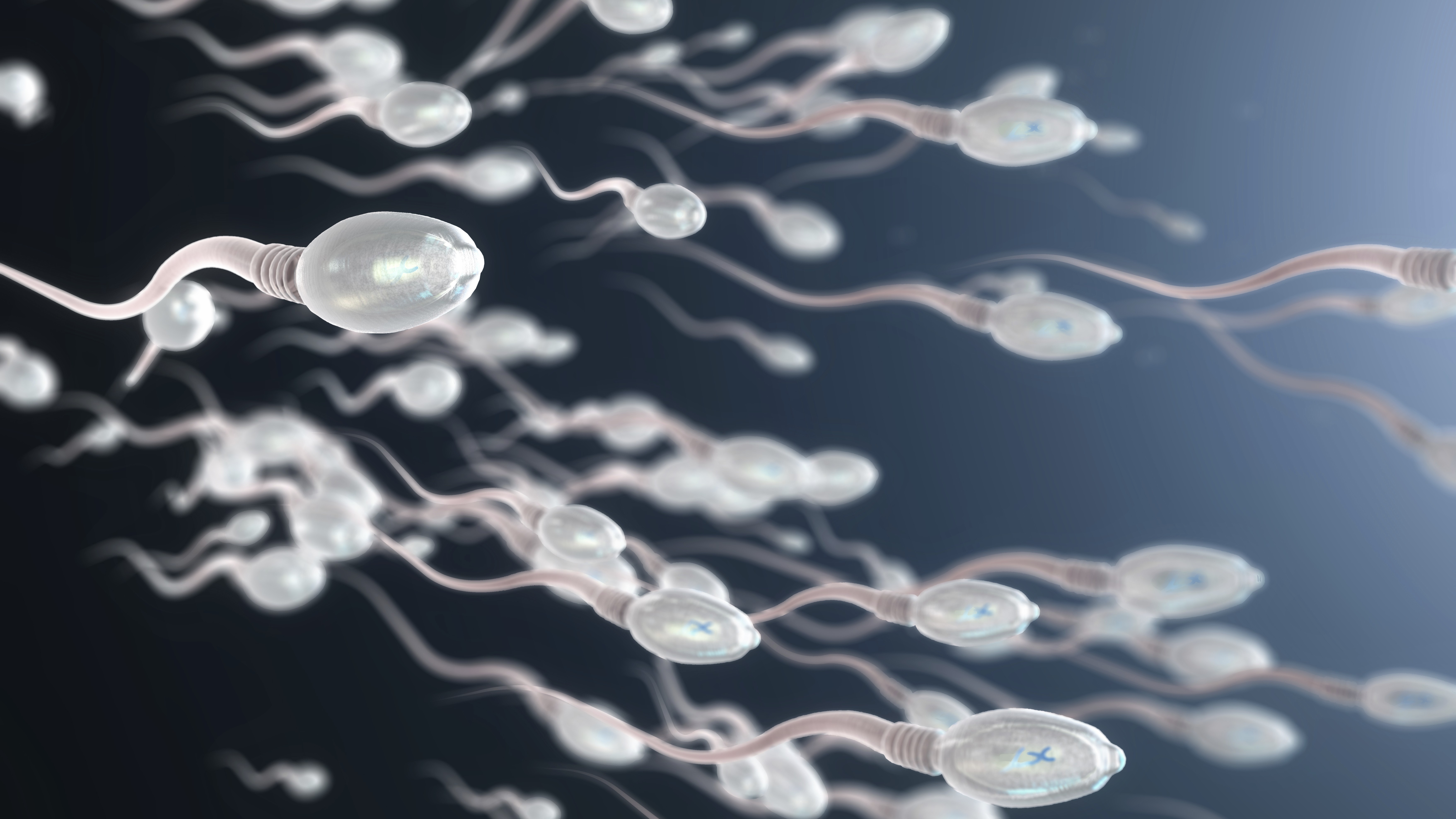
Researchers have created magnetically-controlled “sperm bots” that they can pilot around and monitor in real time.
These tiny microrobots are bull sperm cells coated in magnetic nanoparticles. Researchers haven’t tested them inside a real organism, whether cow or human, yet, but they demonstrated that they can control the sperm bots inside a life-sized anatomical model of the female human reproductive system and track their progress with X-rays.
The sperm bots, described Tuesday (Sep. 2) in the journal npj Robotics, could one day be used to improve reproductive medicine, drug delivery and infertility diagnosis, the researchers said in a statement.
“We’re turning nature’s own cell delivery systems into programmable microrobots,” study lead author Islam Khalil, an associate professor in the robotics and mechatronics research group at the University of Twente in the Netherlands, said in the statement.
Related: ‘I would never let a robot incubate my child’: Poll on ‘pregnancy robots’ divides Live Science readers
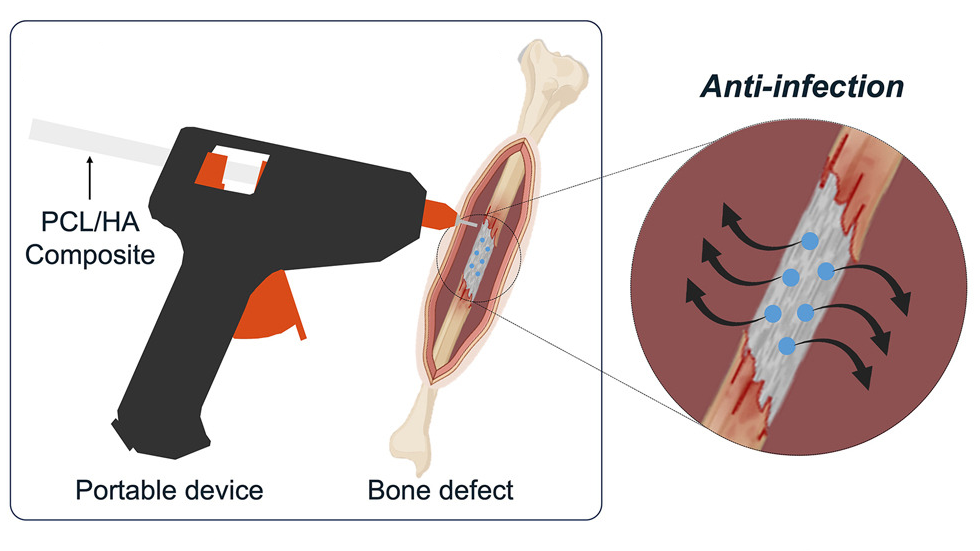
Microbots are microscopic devices that scientists are developing so that they can be deployed inside the body for highly precise, targeted medical treatments. For example, in 2022, researchers used an army of swimming microbots to eradicate a deadly pneumonia infection in mice.
When it comes to reproductive health, scientists say that microbots have the potential to deliver drugs directly to the uterus, fallopian tubes and other difficult-to-access parts of the female reproductive system. Such a targeted drug delivery system could improve treatments for ailments such as uterine cancer and fibroids, the study authors propose.
Khalil was part of a team that unveiled biohybrid magnetic sperm microrobots in 2020. In the new study, researchers found that increasing the concentration of iron oxide nanoparticles on the bots’ outer coating improved the team’s ability to control and detect the little machines, while still ensuring the nanoparticles weren’t harmful to the uterus. At least, the bots weren’t toxic to human uterine cells after 72 hours of exposure.
The team tested their little sperm bots in a 3D printed model of a portion of the female reproductive tract, using an external magnetic field to pilot them from the ersatz cervix, through the uterine cavity, and toward the fallopian tubes, where fertilization most often occurs. They found that the bots could be tracked throughout the journey in real time using X-rays, something that isn’t possible with natural sperm.
“Until now, visualising sperm inside the body was nearly impossible,” Khalil said.
A lack of real-time sperm tracking has hampered scientists’ understanding of reproductive health and fertility treatments, the authors say. The researchers noted that having a noninvasive way of tracking sperm could help them better understand sperm transport systems and male infertility, for instance.