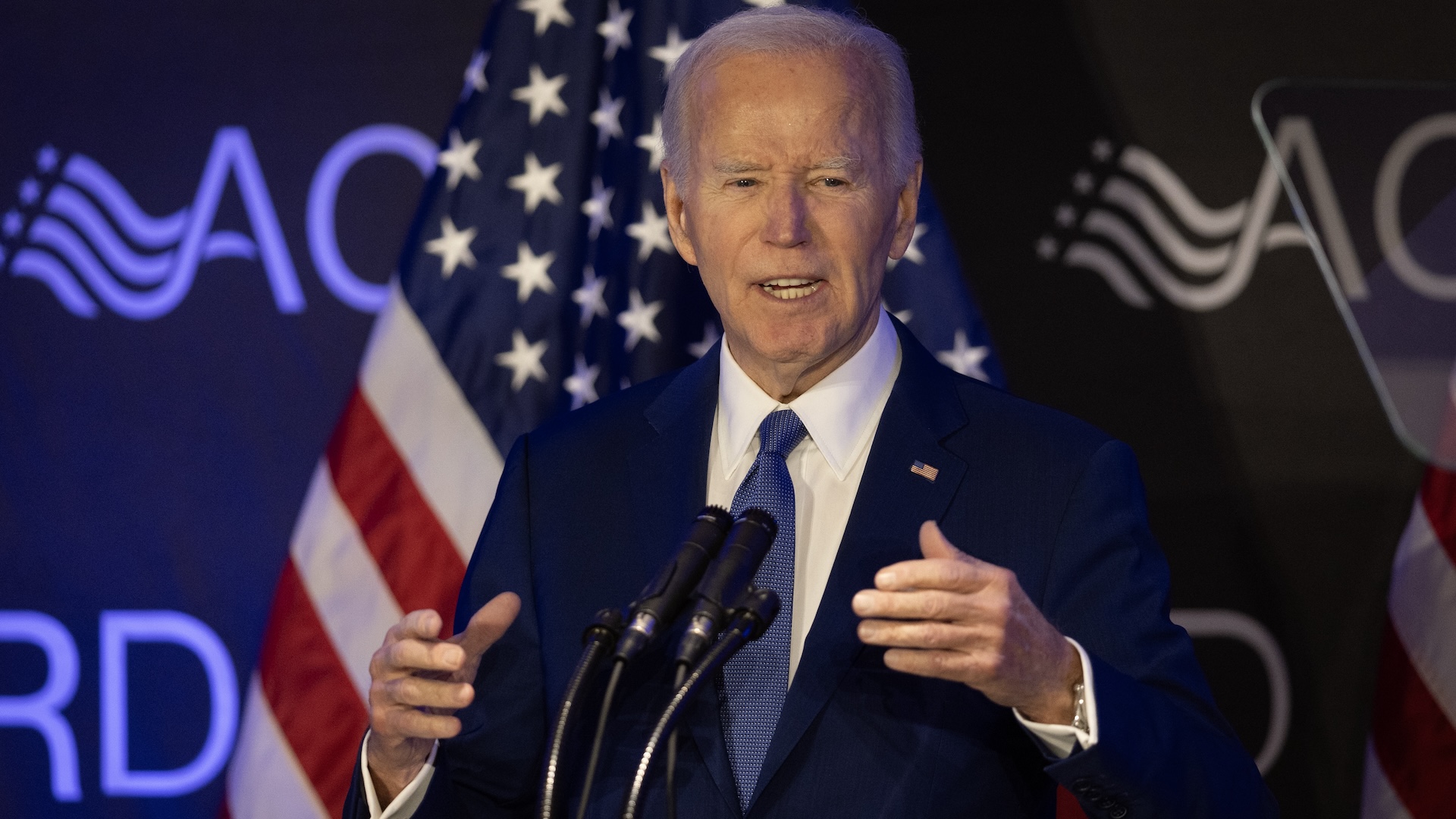
Former President Joe Biden has been diagnosed with an “aggressive” form of prostate cancer, which has spread to his bones, his office announced Sunday (May 18).
The statement noted that Biden, 82, initially experienced urinary symptoms, and on examination, doctors had found a nodule in his prostate. On Friday (May 16), he was diagnosed with prostate cancer. The cancer was “characterized by a Gleason score of 9 (Grade Group 5) with metastasis to the bone,” the statement said, as reported by BBC News. Once prostate cancer has spread to the bones, the survival rate drops significantly.
The severity of prostate cancer is ranked using Gleason scores between 6 and 10, with a higher number meaning that the cancer is more likely to grow quickly and spread to additional body parts, or “metastasize.” These scores help doctors determine how best to treat a given patient’s cancer. “While this [Biden’s score] represents a more aggressive form of the disease, the cancer appears to be hormone-sensitive which allows for effective management,” Sunday’s statement said.
Here’s what to know about prostate cancer, including what determines its severity and how it’s treated.
Related: The 10 deadliest cancers, and why there’s no cure
What is prostate cancer?
Prostate cancer forms in the prostate gland, a small, walnut-sized gland present in males and is located just below the bladder and in front of the rectum. The prostate surrounds part of the urethra, which carries urine out of the bladder. Its main function is to produce and secrete seminal fluid, which forms part of semen.
“Prostate cancer develops when changes in prostate cells lead to uncontrolled growth,” Dr. Justin Stebbing, a professor of biomedical sciences at Anglia Ruskin University, told Live Science via email. “Over time, accumulated DNA errors in prostate cells may turn normal cells into cancerous ones, particularly in those with inherited predispositions or environmental exposures.”
He added that, “factors like aging, family history, and genetic mutations (such as in BRCA genes) play roles.” BRCA genes are perhaps best known because certain mutations in these genes increase breast-cancer risk, but carrying mutations in these genes can also raise the risk of prostate cancer in males.
The growth of prostate cancer cells can be fueled by androgens, meaning male sex hormones like testosterone, Stebbing said, “though not all cases are linked to hormone levels.”
The majority of prostate cancers are adenocarcinomas, which develop in the gland cells lining the prostate and its tubes. A smaller proportion of prostate cancer cases are squamous cell prostate cancers, which affect the cells covering the prostate, and transitional cell carcinomas, which affect the lining of the urethra. A rare type is small cell prostate cancer, which tends to grow much more quickly than other forms.
Prostate cancer is the fourth most common form of cancer globally, and the second most common cancer in men worldwide, according to the World Cancer Research Fund. The U.S. National Institutes of Health estimates that there will be over 300,000 cases in the U.S. in 2025, based on historical trends. Around 1 in 8 men will be diagnosed with prostate cancer during their lifetime, with about 6 in 10 cases diagnosed in men ages 65 or older, according to the American Cancer Society (ACS).
What is the survival rate for prostate cancer?
Prostate cancer survival rates vary with the patient’s age and the aggressiveness of the cancer. Cancer survival rates, in general, are often expressed in terms of five-year relative survival, a measure of the percentage of people who are expected to survive the effects of a given cancer for five years post-diagnosis.
Overall, across all stages of prostate cancer, the five-year survival rate is 97%, according to the ACS. That rate rises to over 99% in cases where the cancer has not spread outside the prostate, or has only spread to nearby structures in the body. However, if the cancer has spread to more-distant parts of the body, such as the bones, liver or lungs, the rate drops to 37%.
“While many prostate cancers grow slowly and have a 5-year survival rate near 100% when localized, advanced cases (where cancer spreads beyond the prostate) are more deadly,” Stebbing said.
What are the symptoms of prostate cancer?
Prostate cancer may not cause symptoms in its early stages. If they do occur, early signs of prostate cancer can include blood in the urine; frequent need to urinate, especially at night; and a weak or interrupted urine flow.
Once the cancer has advanced, and potentially spread to other parts of the body, its symptoms may progress to include erectile dysfunction, weight loss, exhaustion, and weakness or numbness in the legs and feet, due to the tumor pressing onto the spinal cord. It can also cause pain in the hips, back, chest and other body parts, due to cancer having spread into the bones.
What’s the prognosis for prostate cancer that has spread to the bones?
“If prostate cancer spreads to bones (as in advanced cases), it becomes incurable and significantly impacts quality of life,” Stebbing said. “Bone metastases weaken skeletal structure, causing pain, fractures, and complications like spinal cord compression.”
At that stage of the disease, “treatments focus on managing symptoms, slowing progression, and improving survival,” he said. “While newer therapies extend life expectancy, the prognosis remains serious, with median survival around 24 months for spinal metastases.”
Although the statement noted that Biden’s cancer had spread to his bones, it did not note which bones were affected. Dr. Judd Moul, a prostate cancer expert at Duke University, told The New York Times that people whose prostate cancer has spread can potentially live for 10 or more years, depending on the case. Dr. Ryan Cleary, a urologist at MedStar Health, told the BBC that “about a third of patients will still be alive after five years of metastatic prostate cancer.”
Related: Prostate cancer treatments can be avoided or delayed in many cases, huge study finds
What is a Gleason score?
Gleason scores grade prostate cancers on a scale of 6 to 10 based on how abnormal a patient’s cancer cells appear under a microscope. The scores help doctors assess how aggressive the cancer is, meaning how quickly it is likely to grow and how likely it is to spread.
“The Gleason grading system allows us to consider how much the cells within the tumour have changed, compared to how they should look,” Dr. Michael Porter, a senior lecturer in medicine and molecular genetics at the University of York in the U.K., told Live Science via email. “A small amount of tissue (biopsy) is taken from the tumour and looked at under a microscope.”
This system involves looking at two different regions of the tumor and rating how abnormal the cells appear in each region. These initial grades run 1 through 5, from most normal-looking to most abnormal-looking, and then the two grades are added together to produce the final Gleason score.
Gleason scores of 6 indicate that a cancer is likely low risk, while Biden’s Gleason score of 9, would suggest that cells are extremely abnormal and are likely to grow quickly and spread elsewhere.
What does “hormone sensitive” mean?
While Biden’s cancer is reportedly aggressive and has already spread to his bones, his office also noted in the statement that the cancer was “hormone-sensitive.” That means that the cancer cells rely on male sex hormones (androgens), such as testosterone and dihydrotestosterone (DHT), to grow. Hormone-sensitive cancers can be targeted with treatments that lower these hormone levels or block their activity.
“This type of cancer is usually highly dependent on the presence of the hormone testosterone, to survive and develop,” Porter told Live Science. “So, by depriving them of the hormone, the development of the cancer can hopefully be slowed or reversed.”
These hormone treatments can include drugs that reduce testosterone levels in the body; drugs that block testosterone from binding to cancer cells; or even surgical removal of the testes, the organs that produce androgens.
“As [Biden’s] prostate cancer is apparently hormone sensitive, it is far easier to treat the whole body, targeting all the potential sites the cancer could have moved to,” Porter said. “In cancers where the treatment is more localised, this can be a more difficult thing to do.”
Androgen-depleting treatments can have some side effects. “These can potentially include an increase in the size of the breast, hot flushes, an increase in body fat and impotence,” Porter said. Additionally, these hormone treatments can become less effective over time, as the cancer cells find ways to grow without sex hormones.
“Most cancers eventually become resistant to such treatments, entering a ‘castration-resistant’ phase where alternative approaches are needed,” Stebbing said. “Early hormone-sensitive stages often respond well to targeted therapies, delaying progression.”
Prostate cancer is also commonly treated using radiation therapy and surgical removal of the prostate, but prostate removal isn’t typically used in people whose cancer has already spread to the bones. Again, prostate cancer that has spread to the bones cannot typically be cured, but the ACS notes that there are treatments that can inhibit further spread and improve quality of life.
This article is for informational purposes only and is not meant to offer medical advice.