Germ theory was never a given. This now-commonplace idea — the notion that human diseases can be sparked by tiny pathogens infiltrating the body — emerged on the backs of discoveries made by people over time. Those discoveries steadily slotted together to form a bigger picture, revealing both the wonders and terrors of the microbial world around us.
Thomas Levenson, a professor of science writing at MIT and author, traces the history of germ theory from its inception to the present day in a new book called “So Very Small: How Humans Discovered the Microcosmos, Defeated Germs — and May Still Lose the War Against Infectious Disease” (Random House, 2025). In the book, Levenson also tackles the larger question of how and why new ideas are pursued, accepted or ignored.
In the following passage from “So Very Small,” he highlights how, despite our modern understanding of germs, we’re still locked in an ongoing struggle with them and with our own hubris. The rise of antibiotic-resistant superbugs is a prescient example of that, he argues.
Related: Superbugs are on the rise. How can we prevent antibiotics from becoming obsolete?
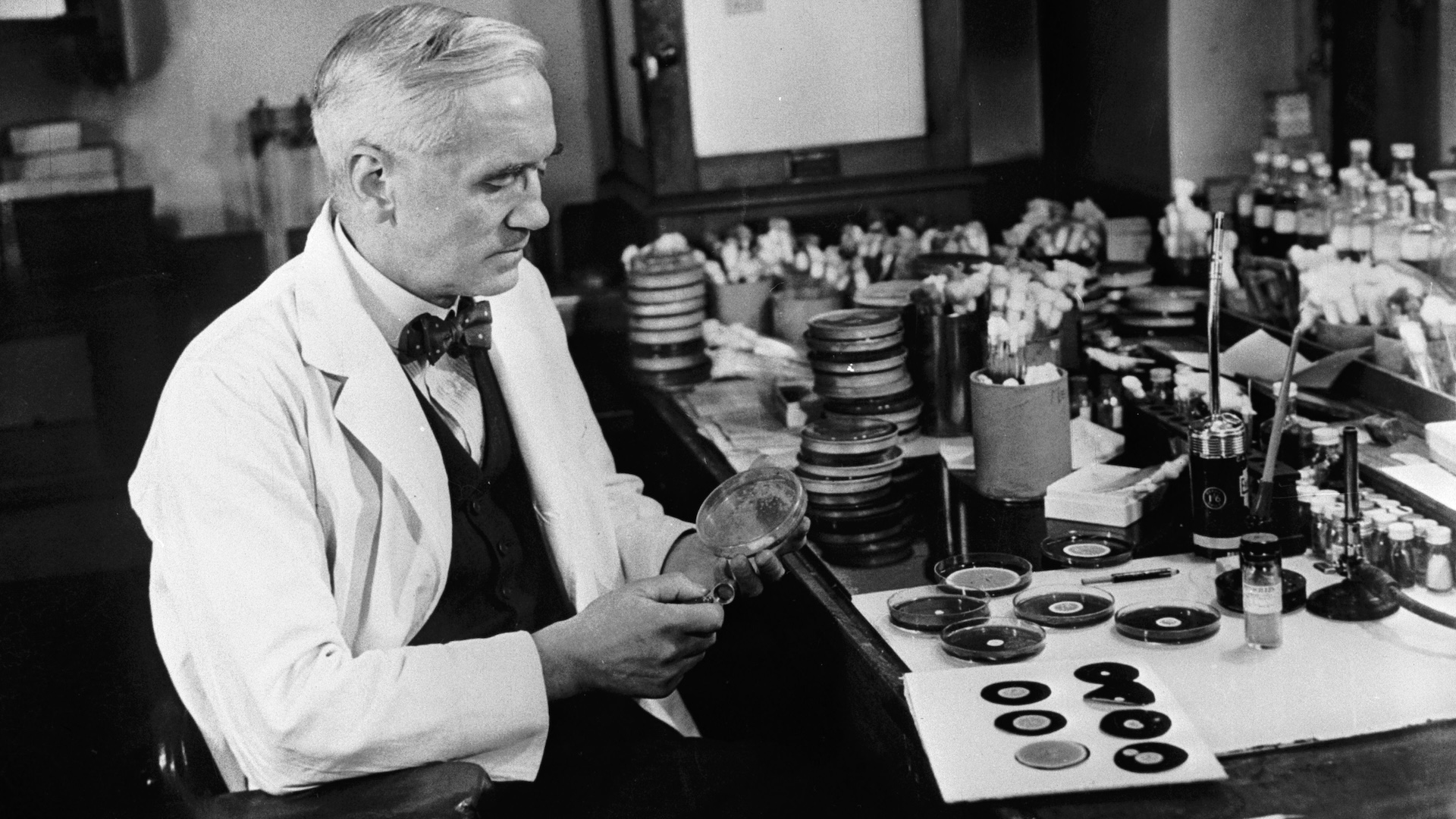
Autumn, 1945. The war in Europe has been over for five months. Something resembling normal life is sputtering into shape. In Stockholm, for the first time since 1938, the Nobel Foundation is getting ready to award its full catalog of prizes. The deliberations reach a familiar intensity as the committees for each scientific discipline struggle to apportion credit to no more than three people for discoveries to which dozens or more had contributed. Finally, on October 25, telegrams go out to the winners of the Nobel Prize for Physiology and Medicine: Alexander Fleming for discovering penicillin, and Howard Florey and Ernst Chain
for turning Fleming’s mold juice into a world-changing medicine.
The prize ceremony takes place on December 10. At the traditional after-party there is plenty of drink on tap, and rumors of dancing. The usually buttoned-down Fleming keeps going until three a.m. The next day, hungover or not, the three new laureates deliver their Nobel lectures. Fleming goes first, devoting most of his talk to retelling the details of his serendipitous encounter with the penicillium mold. As he draws to a close, though, he abandons memory to deliver a sermon, complete with the command that his audience go forth and sin no more:
“The time may come when penicillin can be bought by anyone in the shops. Then there is the danger that the ignorant man may easily underdose himself and by exposing his microbes to non-lethal quantities of the drug make them resistant. Here is a hypothetical illustration. Mr. X has a sore throat. He buys some penicillin and gives himself, not enough to kill the streptococci but enough to educate them to resist penicillin. He then infects his wife. Mrs. X gets pneumonia and is treated with penicillin. As the streptococci are now resistant to penicillin the treatment fails. Mrs. X dies. Who is primarily responsible for Mrs. X’s death? Why Mr. X whose negligent use of penicillin changed the nature of the microbe. Moral: If you use penicillin, use enough.”
This was no mere parable. What Fleming prophesied as he stood before Sweden’s great and good had already come to pass. The first of four cases of gonorrhea “resistant to ‘large’ amounts of penicillin” appeared in the medical literature in 1946. Even earlier, as far back as 1940, Edward Abraham and co-workers in Florey’s laboratory had been able to train cultured colonies of staphylococcus to resist penicillin in their petri dishes. And, of course, the wartime erosion of the effectiveness of sulfa drugs against gonorrhea was a very public demonstration of the problem.
And yet, despite Fleming’s warning, the dynamic that killed Mrs. X has recurred again and again throughout the antibiotic era. The first drug effective against TB, streptomycin, was isolated in 1944. Resistant strains of M. tuberculosis emerged no later than 1948. It’s been the same story in disease after disease, bug after bug, drug to drug to drug. Staphylococcus aureus, the ubiquitous killer of World War I’s wounded, has shrugged off penicillin, erythromycin, the tetracyclines, and what was seen as the big gun, methicillin.
Related: Dangerous ‘superbugs’ are a growing threat, and antibiotics can’t stop their rise. What can?
Methicillin came on the market in 1959. Its effectiveness began to erode almost immediately. The first staph strain immune to the new drug showed up later in 1961, marking the appearance of what we now know as MRSA, or Methicillin-resistant Staphylococcus aureus. MRSA flourishes in hospitals, where microbes and plentiful antibiotics meet, but over time has emerged in the broader population. This pattern has been repeated across the spectrum of diseases around the world. About 1.3 million people die of TB each year. As of 2020, XDR-TB, extensively drug-resistant tuberculosis, has been reported in 123 nations. For those infected with XDR-TB, all front-line antibiotics have failed, along with at least one of the three break-glass-in-case-of-emergency backup drugs.
Taken together, there were nearly 3 million antibiotic-resistant infections in the United States in 2019, the most recent numbers available as of this writing. Some 35,000 Americans died that year of once-treatable microbial diseases. Since 1945, we have failed both to anticipate the speed with which microbes would gain the ability to evade our best drugs, and to come up with a satisfactory response to their resistance — to the point where the single greatest gift of germ theory may not be wholly ours much longer.
Shards of that future are already here. What are sometimes called superbugs — microbes resistant to every available drug — are not merely the stuff of nightmares. They are taking lives right now. A report published by the U.S. Centers for Disease Control and Prevention described the case of a woman in her seventies who had been traveling across the Indian subcontinent. They did not release her name but reported that somewhere on her travels she fractured her femur. She was taken to one hospital, then another, and then on to more in India. In August 2016, she returned to her home in Washoe County, Nevada. She went back to the hospital, presenting with systemic inflammatory response syndrome, a characteristic immune response to an unresolved infection. So her doctors looked for the microbe that could have engendered her increasingly perilous condition.
They found it in Klebsiella pneumoniae, a bacterium that occurs naturally in soils and can live quite peaceably in human guts, mouths, or skin. If it makes its way elsewhere, though, it can cause disease, often pneumonia, but several other conditions as well. Until recently, treating a K. pneumoniae infection was simple. Any one of several common antibiotics could do the job. So her medical team tested the patient’s bacterial samples to see which drug would be most effective. The answer came back: none of them. The woman’s microbes were resistant to the fourteen antibiotics available in Reno. The hospital sent samples to the federal Centers for Disease Control and Prevention, and the tests there showed that these bugs were resistant to twelve more medicines — which is to say, all the remaining possibilities. There was nothing available in the United States that could knock out her singular infection.
Within weeks the woman was dead, slain by a superbug for which there was no cure. She wasn’t the first such casualty and she certainly has not been the last. But this one life lost to an infection that so recently was trivially easy to cure forces the question: How could this happen? How could it have been allowed to happen?